Therapy with the TheraBionic P1
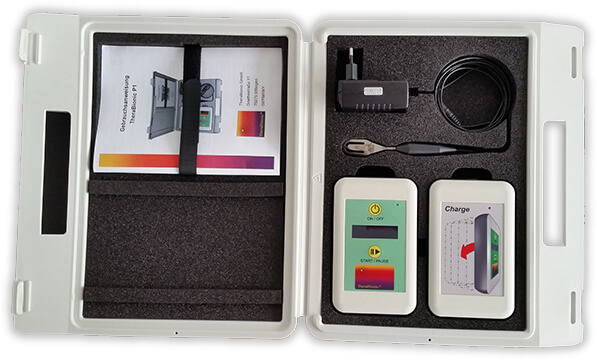
The TheraBionic P1 device
The TheraBionic P1 produces low levels radiofrequency (RF) electromagnetic fields, which are amplitude-modulated at tumor-specific frequencies. The device is coupled with a spoon-shaped antenna, which is placed in the patient’s mouth, more precisely on the anterior part of the patient’s tongue for three sixty-minute sessions per day. When the spoon-shaped antenna is placed on the patient’s tongue, it delivers low levels of radiofrequency electromagnetic fields throughout the patient’s body.
The TheraBionic P1 emits low levels of radiofrequency electromagnetic fields and the levels delivered during treatment are lower than those generated by cellular phones when held close to the body. No serious adverse events have ever been reporting with the use of the TheraBionic P1 device, even after more than six years of continuous use.
Until recently, only symptomatic treatment was advised for patients who have failed or are intolerant to first line and second line therapies for advanced hepatocellular carcinoma.
The TheraBionic P1 device enables a new and innovative treatment approach. It is used for the systemic treatment of patients with advanced hepatocellular carcinoma who have either failed first and second line therapies or are intolerant of first and second line therapies.
In an investigator-initiated, single-group, single-center, non-randomized, phase I/II study in patients with advanced HCC, Costa and collaborators assessed the safety and effectiveness of treatment of advanced hepatocellular carcinoma with HCC-specific modulation frequencies of low energy radiowaves.(Costa, de Oliveira et al. 2011)
Patients with advanced HCC with or without metastases, diagnosed by imaging or biopsy, age 18 years or older with an ECOG performance status of 0 to 2 and with permanently impaired liver function were eligible for enrollment. Previous local or systemic treatments with sorafenib or chemotherapy were allowed. Forty-one patients with advanced HCC and Child Pugh A or B disease and limited therapeutic options received intervention (6 females, 35 males; median age: 64 years; range: 18 – 85; BCLC status B: n=6, BCLC status C: n=35). Thirty-one patients (75.6%) had radiological evidence of disease progression at the time of enrollment as defined by comparison of baseline imaging studies with imaging studies obtained within the previous six months. Thirty-four (82.9%) patients had received therapy prior to enrollment, 25 of them chemoembolization. Seven (17.1%) patients had not received therapy prior to enrollment because of (1) severely impaired liver function in five cases, or (2) refusal to receive chemotherapy for metastatic disease.
The HCC treatment program consisted of sequential emission of repeated cycles of 194 HCC-specific modulation frequencies identified by the methods described in Barbault et al.(Barbault, Costa et al. 2009) for 60 min, three times daily. Treatment with the device was administered until disease progression or death. Imaging studies were performed every 8 weeks. Patients were treated in two sequential cohorts. After the first cohort (n=23) showed encouraging results (Progression-free survival ≥ 6 months: n = 6), the second cohort (n=18) was enrolled.
The primary end point was the proportion of patients who were progression-free at 6 months. Secondary end points were median progression-free survival (PFS) (first day of treatment until progression of disease or death) and median overall survival (OS) (first day of receiving treatment to death).
Treatment efficacy
Of the 41 patients, 14 patients (34.1%) had stable disease (SD) for more than 6 months, which met the preplanned primary efficacy criterion of 8 patients with progression-free survival of at least 6 months. Median progression-free survival was 4.4 months (95% CI 2.1–5.3) and median OS was 6.7 months (95% CI 3.0–10.2). Estimated survival at 12, 24 and 36 months was 27.9% (s.e. = 7.1%), 15.2% (s.e. = 5.7%), and 10.1% (s.e. = 4.8%), respectively. Overall, there were six long-term survivors with an OS greater than 24 months and four long-term survivors with an OS greater than 3 years. Importantly, five of the six (83%) long-term survivors had radiological evidence of disease progression at the time of study enrolment. Two of three patients with the longest survival (44.6 and +58 months) had radiological evidence of disease progression at the time of enrolment, and BLCL stage C disease. The latter patient remained on therapy with a near complete response for 58 months.
Tumour shrinkage
Tumor shrinkage as assessed by radiological imaging as well as changes in AFP levels were documented in patients with advanced HCC receiving RF EMF modulated at HCC-specific frequencies administered by the intrabuccal probe. Antitumor activity in patients with advanced HCC was exemplified by partial responses observed in four patients (9.8%) and decreases in AFP levels greater than 20% in four patients. A total of 18 patients (43.9%) either had objective response or SD for greater than 6 months. Importantly, clinical benefit also was observed in patients with Child Pugh B disease, i.e., patients with severely impaired liver function who tolerate poorly antitumor treatment with drugs such as sorafenib (Nexavar®), Lenvatinib (Lenvima®) or regorafenib (Stivarga®).
Symptomatic benefit
In all, 11 patients reported pain before treatment initiation, 3 patients reported grade 3, 5 patients reported grade 2, and 3 patients grade 1 pain. After initiation of treatment, five (45.5%) patients reported complete disappearance of pain and two (18.2%) patients reported decreased pain. Two patients reported no changes and two patients reported increased pain. Hence, 63.6% of patients with cancer-related pain experienced symptomatic benefit.
Comparison with phase II study on Sorafenib
These results were compared with results by Abou-Alfa et al.(Abou-Alfa, Schwartz et al. 2006): In a large phase II study assessing the effects of Sorafenib in patients with HCC and Child–Pugh A and B who had not received previous systemic treatment, Abou-Alfa et al. observed partial responses using the WHO criteria in 2.2% of patients. This compares to 9.8% with the TheraBionic device, which is an about fourfold higher percentage. Investigator-assessed median time to progression in the Sorafenib study was 4.2 months, and median OS was 9.2 months. Of note, all 137 patients from that study had evidence of disease progression after 14.8 months. At the same time point, four (9.8%) of the patients enrolled in the TheraBionic study did not have evidence of disease progression. These findings suggest that the TheraBionic device may increase the time to radiological progression in advanced HCC. Importantly, the ratio of Child-Pugh A patients vs. Child-Pugh B patients was higher in the Abou-Alpha et al. study(Abou-Alfa, Schwartz et al. 2006) than in the Costa et al. study.(Costa, de Oliveira et al. 2011) Thus, better outcome in the Costa et al. study cannot, therefore, be attributed to better general physical condition.
Mechanism of action of frequencies on HCC

In 2001 Pasche and Barbault began examining patients with a diagnosis of cancer with the goal of identifying cancer specific frequencies. Using noninvasive devices emitting very low and safe levels of radiofrequency electromagnetic fields, commonly named radiowaves, they discovered that patients with a diagnosis of cancer exhibited subtle but reproducible changes in their palpable pulse when exposed to certain frequencies. Next, they hypothesized that the frequencies they had discovered could be used to treat cancer and designed a study in which patients were offered treatment with tumor-specific frequencies. Radiowaves modulated at the tumor-specific frequencies were delivered for three hours daily by means of a battery-operated portable device connected to a spoon-shaped antenna placed on the patient’s tongue, which results into the delivery of radiowaves throughout the body.(Barbault, Costa et al. 2009)

Several patients enrolled in this study, published in 2009, had evidence of either tumor shrinkage or stabilization of the growth of the tumor, confirming the hypothesis that radiowaves modulated at specific tumor frequencies could block cancer growth.(Barbault, Costa et al. 2009) This hypothesis was further confirmed in a subsequent study conducted by Costa and collaborators in patients suffering from advanced hepatocellular carcinoma, which was published in 2011.(Costa, de Oliveira et al. 2011) In that study, treatment with the cancer-specific radiowaves again resulted in either tumor shrinkage or tumor growth arrest in approximately half of the patients treated.(Costa, de Oliveira et al. 2011)

In 2012, Zimmerman and collaborators working in Pasche’s laboratory demonstrated that the cancer-specific radiowaves identified in patients with a diagnosis of cancer were able to block or slow down the growth of cancer cells. These experiments were conducted with laboratory equipment replicating the same radiofrequency levels as those generated in patients receiving treatment with the portable device connected to the spoon-shaped antenna. These experiments also showed that the growth of cancer cells was only blocked when tumor-specific radiowaves were used, i.e. HCC-specific radiowaves blocked the growth of HCC cells but did not affect the growth of breast cancer cells. Similarly, breast cancer-specific radiowaves blocked the growth of breast cancer cells but did not affect the growth of HCC cells. Additionally, radiowaves chosen at random did not affect the growth of any cancer cells thus confirming the well accepted concept that randomly-chosen radiowaves such as those generated by devices such as cellular phones do not affect the growth of cancer cells or normal cells.
Comparison with the results from randomized studies conducted in patients with advanced hepatocellular carcinoma
The following report describes a methodologically sound assessment of the therapeutic efficacy of the TheraBionic (TB) device by way of a statistical analysis of several studies. In this report the results of a single arm TheraBionic study are compared with control groups and treatment groups from two other studies. We examine three outcomes:
- Progression Free Survival
- Response Rate
- Overall Survival Among Patients who are not Child Pugh Class B
The data from this analysis derives from three studies on hepatocellular carcinoma that were published in major scientific journals:
- Costa FP et al (2011) Treatment of advanced hepatocellular carcinoma with very low levels of amplitude-modulated electromagnetic fields, British Journal of Cancer 105, 640-648(Costa, de Oliveira et al. 2011)
- Bruix J et al, (2017) Regorafenib for patients with hepatocellular carcinoma who progressed on sorafenib treatment (RESORCE): a randomized, double-blind, placebo-controlled, phase 3 trial, Lancet 389:56-66(Bruix, Qin et al. 2017)
- Zhu AX, et al (2015) Ramucirumab versus placebo as second-line treatment in patients with advanced hepatocellular carcinoma following first-line therapy with sorafenib (REACH): a randomized, double-blind, multicenter, phase 3 trial Lancet Oncology 16:859-70(Zhu, Park et al. 2015)
The following comparisons were made by way of statistical analyses:
- Comparing the TheraBionic efficacy results to the placebo groups in the Bruix and Zhu studies
- Progression free survival (PFS) for all patients
- Response rate for all patients
- Overall survival removing Child Pugh Class B patients from the TheraBionic group
- Comparing the TheraBionic efficacy results to the regorafenib arm in the Bruix study. No comparison was made with ramucirumab since the Zhu study did not show any significant difference between the ramucirumab and placebo.
- Progression free survival for all patients
- Response rate for all patients
- Overall survival removing Child Pugh Class B patients from the TheraBionic group
Results Placebo
Progression Free Survival - TheraBionic vs Placebo
TheraBionic (TB) vs Placebo in Bruix paper
| Study | Median PFS | Lower 95% Confidence Limit | Upper 95% Confidence Limit |
| TB(treatment group) | 4.4 months | 2.1 months | 5.3 months |
| Bruix(placebo group) | 1.5 months | 1.4 months | 1.6 months |
The 95% confidence intervals from these two studies do not overlap – in fact, the difference between the upper bound for the Bruix study and the lower bound for the TheraBionic study is 0.5 months. This provides very robust evidence that the progression free survival (PFS) for patients in the TheraBionic study is statistically superior to the placebo group in the Bruix study.
TheraBionic (TB) vs Placebo in Zhu paper
| Study | Median PFS | Lower 95% Confidence Limit | Upper 95% Confidence Limit |
| TB | 4.4 months | 2.1 months | 5.3 months |
| Zhu | 2.1 months | 1.6 months | 2.7 months |
The 95% confidence intervals from these two studies overlap by 0.6 months, however the upper bound for the placebo group in the Zhu study is 1.7 months less than the median PFS in the TB study (2.7 months vs 4.4 months). Furthermore, the observed median in the TheraBionic study is 2.09 times longer than the observed median in the Zhu study. In the Zhu paper, the authors reported that a 0.7 month (2.1 vs 2.8 month) improvement in PFS resulted in a highly significant difference between groups (p<0.0001, Figure 3A in the paper). Conclusion: the present data comparison strongly supports the determination that the PFS rate in the TB patients is statistically superior to the PFS rate in the placebo group in the Zhu paper.
The above two analyses support the assertion that Progression Free Survival is significantly improved for patients who are treated with the TheraBionic device when compared with placebo (standard of care after sorafenib failure) patients.
Response Rate TheraBionic vs Placebo
TheraBionic (TB) vs Placebo in Bruix paper
| Study | Response Rate (CR+PR) | Lower 95% Confidence Limit (Exact Confidence Interval) | Upper 95% Confidence Limit(Exact Confidence Interval) |
| TB | 4/41 = 9.76% | 2.7% | 23.1% |
| Bruix | 8/192 = 4.1% | 1.8% | 7.96% |
The observed response rate in the TheraBionic group is 2.4 times higher than the response rate in the Bruix placebo group. In addition, the upper bound of the confidence interval for the placebo group is lower than the observed response rate in the TheraBionic group. Finally, a one sample Binomial test for whether the TheraBionic response rate is 4.1% (Null Hypothesis base on Placebo rate) versus the one-sided alternative that the TheraBionic response rate is superior to the Placebo rate has a p-value of 0.034.
TheraBionic (TB) vs Placebo in Zhu paper
| Study | Response Rate (CR+PR) | Lower 95% Confidence Limit (Exact Confidence Interval) | Upper 95% Confidence Limit(Exact Confidence Interval) |
| TB | 4/41 = 9.76% | 2.7% | 23.1% |
| Zhu | 2/282 = 0.7% | 0.9% | 2.5% |
The 95% confidence intervals from these two studies do not overlap. This is very robust evidence that the true response rate in the TheraBionic group is superior to the observed response rate in the Zhu placebo patients. Furthermore, a one-sample binomial test for whether the TheraBionic response rate is 0.7% (Null Hypothesis base on Placebo rate) versus the one-sided alternative that the TB response rate is superior to the Placebo rate has a p-value less than 0.0001.
The two analyses provide solid statistical evidence that Progression Free Survival is significantly improved for patients who are treated with the TheraBionic device when compared with placebo (standard of care after sorafenib failure) patients.
Overall Survival of TheraBionic Patients who are not Child Pugh Class B vs Placebo
Prior to performing this analysis Child Pugh Class B patients were removed from the TheraBionic study group. This was done because the TheraBionic study contained significantly more patients in this group than the Placebo group in both the Bruix and Zhu studies. In the TheraBionic study there were 20/41 (49%) of patients with Child Pugh Class B status, whereas in the Bruix study there were 6/194 (3%) and in the Zhu study there were 6/282 (2%). Patients were required to have Child Pugh A liver function in these two studies. However, those patients in the Bruix and Zhu studies who progressed to Child Pugh B after screening and before randomization were included. Since patients in this group (Child Pugh Class B) are known to have a worse survival prognosis than patients with Child Pugh Class A, these patients were removed.
TheraBionic vs Placebo in Bruix paper
| Study | Median OS | Lower 95% Confidence Limit | Upper 95% Confidence Limit |
| TB | 9.8 months | 4.4 months | 27.1 months |
| Bruix | 7.8 months | 6.3 months | 8.8 months |
The observed median OS in the TheraBionic group is 2 months higher than the placebo median OS. Furthermore, the upper bound of the 95% confidence interval for the placebo group is 8.8 months which is one month lower than the observed median OS in the TheraBionic group. This is solid statistical evidence that OS is longer in the TheraBionic group than the Placebo group
TheraBionic vs Placebo in Zhu paper
| Study | Median OS | Lower 95% Confidence Limit | Upper 95% Confidence Limit |
| TB | 9.8 months | 4.4 months | 27.1 months |
| Zhu | 7.6 months | 6.0 months | 9.3 months |
The observed median OS in the TheraBionic group is 2.2 months higher than the placebo median OS. Furthermore, the upper bound of the 95% confidence interval for the placebo group is 9.3 months, which is ½ month lower than the observed median OS in the TheraBionic group. This is solid statistical evidence that OS is longer in the TheraBionic group than the Placebo group.
These two analyses provide solid statistical evidence that the Overall Survival rate in the placebo patients is between 7.6 and 7.8 months. Since these two studies had nearly identical observed medians and comparable 95% confidence intervals there is evidence that the OS rate in placebo patients is in the observed range of these studies. The TheraBionic OS rate is 2 months higher than the placebo group OS rate (from both studies) and the upper bound for this interval is over 2 years (27.1 months).
Summary of TheraBionic comparisons to Placebo groups
For each of the three outcomes presented there is very strong statistical evidence in support of the assertion that the TheraBionic therapy provides statistically significant improvement in clinically meaningful outcomes (Progression Free Survival, Response Rate and Overall Survival) when compared to placebo data from two large contemporary Phase 3 trials with 476 total placebo patients.
Results Regorafenib
Response Rate TheraBionic vs Regorafenib (Bruix paper)
Response Rate TheraBionic vs Regorafenib (Bruix paper)
| Study | Response Rate (CR+PR) | Lower 95% Confidence Limit (Exact Confidence Interval) | Upper 95% Confidence Limit(Exact Confidence Interval) |
| TB | 4/41 = 9.76% | 2.7% | 23.1% |
| Bruix | 40/379 = 10.5% | 7.7% | 14.1% |
The observed response rate in the TheraBionic group is less than 1% lower than the response rate in the Bruix Regorafenib group. In addition, the confidence intervals overlap well, suggesting that the two response rates are very comparable.
Response Rate TheraBionic vs Regorafenib (Bruix paper)
Response Rate TheraBionic vs Regorafenib (Bruix paper)
| Study | Response Rate (CR+PR) | Lower 95% Confidence Limit (Exact Confidence Interval) | Upper 95% Confidence Limit
(Exact Confidence Interval) |
| TB | 4/41 = 9.76% | 2.7% | 23.1% |
| Bruix | 40/379 = 10.5% | 7.7% | 14.1% |
The observed response rate in the TheraBionic group is less than 1% lower than the response rate in the Bruix Regorafenib group. In addition, the confidence intervals overlap well, suggesting that the two response rates are very comparable.
Overall Survival of TheraBionic Patients who are not Child Pugh Class B vs Regorafenib Patients
As described above, prior to performing this analysis Child Pugh Class B patients were removed from the TheraBionic study group. This was done because the TheraBionic study contained significantly more patients in this group than the Regorafenib group in the Bruix study. In the TheraBionic study there were 20/41 (49%) of patients with Child Pugh Class B status, whereas in the Bruix study there were 6/379 (1.6%). Since patients in this group (Child Pugh Class B) are known to have a worse survival prognosis than patients with Child Pugh Class A disease, these patients were removed.
Overall Survival of TheraBionic Patients who are not Child Pugh Class B vs Regorafenib Patients
| Study | Median OS | Lower 95% Confidence Limit | Upper 95% Confidence Limit |
| TB | 9.8 months | 4.4 months | 27.1 months |
| Bruix | 10.6 months | 9.1 months | 12.1 months |
The observed median OS in the TheraBionic group is 0.8 months lower than the Regorafenib median OS. This value is well within the 95% confidence interval for the Regorafenib group and thus provides evidence that the OS time is not significantly different between the TB and Regorafenib groups.
Summary of TB comparison to Regorafenib Group
For PFS, TheraBionic was slightly better than the Regorafenib group (1.3 months) and for the Response Rate and OS TB was slightly lower than the Regorafenib group (0.74% lower and 0.8 months shorter).
These analyses provide statistical evidence to support the assertion that the TheraBionic therapy produces comparable (i.e. non-inferior) results when compared to Regorafenib patients in clinically meaningful outcomes (Progression Free Survival, Response Rate and Overall Survival) from a large contemporary Phase 3 trial with 379 Regorafenib patients.
Overall Conclusions of the statistical evaluation of the single arm
TheraBionic study compared with control groups and treatment groups from two other studies assessing the efficacy of new drugs as second line treatment of advanced hepatocellular carcinoma.
Since the pivotal patient trial evaluating the TheraBionic device was conducted using a single-arm design there was a question as to the robustness of the clinical efficacy findings if they were compared to appropriate control group populations. The analyses provided above demonstrate that the TheraBionic device shows statistically significant improvement in clinically meaningful outcomes of PFS, OS and Response Rate when compared to two separate control group populations. This evidence should be considered as very strong since these findings are supported by two different Phase 3 control group populations. In addition, the analyses above provide evidence to suggest that the TheraBionic device is not inferior to the Regorafenib therapy and, depending on the outcome, may be better than that therapy. Finally, it is important to recognize that 20/41 (48.9%) of patients in the TheraBionic study received clinical benefit from receiving this therapy (PR+SD) even though the patients enrolled in the TheraBionic study were very high risk (49.8% with Child Pugh Class B at the time of enrolment) and thus had very poor prognosis for response or survival.
In conclusion, data from the contemporary published literature provide compelling evidence to support the efficacy of the TheraBionic therapy in patients with advanced hepatocellular carcinoma.
Conclusions
Treatment with intrabuccally administered amplitude-modulated electromagnetic fields is safe, well tolerated, and shows evidence of clinical benefit, i.e. anti-tumor effects and symptomatic benefit, in patients with advanced hepatocellular carcinoma who have no other therapeutic option available. The majority of patients enrolled in this study had either failed standard treatment options or had severely impaired liver function that limited their ability to tolerate any form of systemic or intrahepatic therapy. Indeed, 16 patients (39.0%) had Child–Pugh B8 or B9 disease. Among these patients, the median progression-free survival was 4.4 months (95% CI 1.6–7.6 months), which is identical to that of the entire group. Five of these 16 patients (31.3%) received therapy for more than 7.5 months, which indicates that this therapy is well tolerated even in patients with severely impaired liver function.
Complications
Treatment was well tolerated and there was no NCI grade 2, 3 or 4 toxicities despite long-term treatment. The only treatment-related adverse events were grade 1 mucositis (one patient) and grade 1 somnolence (one patient) over a total of 266.8 treatment months.
